Subtotal $0.00
When we think about heart health, we often focus on diet, exercise, and lifestyle choices. But what if I told you that your mental health plays a crucial role, too? The relationship between heart disease and mental well-being is more intertwined than we might realize. Anxiety and depression don’t just affect our mood; they can also have a significant impact on our heart health.
Managing these mental health challenges is essential not just for our emotional resilience but also for keeping our hearts in peak condition. Let’s dive into this important link and explore practical ways to handle anxiety and depression, paving the way for a healthier heart and a happier mind.
Heart disease and mental health are interconnected in significant ways that may not be immediately apparent. Individuals managing heart conditions frequently experience anxiety and depression, which can impede their recovery and overall quality of life. Conversely, those with mental health disorders often face an increased risk of developing cardiovascular issues.
In this discourse, we will examine the compelling relationship between heart disease and mental health. We will elucidate how cardiovascular conditions can influence psychological well-being and will present practical, evidence-based strategies aimed at enhancing both mental and physical health. We invite you to join us as we explore the essential connection between cardiovascular health and mental wellness.
Understanding the Relationship Between Cardiovascular Disease and Mental Health
The Mind-Heart Connection
The relationship between mental health and cardiovascular health is highly bidirectional. Emotional stressors can significantly contribute to developing heart conditions, while living with a cardiovascular diagnosis can increase the risk of experiencing mental health challenges, such as anxiety and depression. This interconnectedness highlights the importance of addressing both psychological and physical health in comprehensive care.
The Impact of Anxiety on Cardiovascular Health
Chronic anxiety activates the body’s fight-or-flight response, releasing stress hormones like cortisol and adrenaline. These hormones raise heart rate, increase blood pressure, and promote inflammation, each serving as a key risk factor for cardiovascular disease. In addition, unhealthy coping mechanisms, including smoking and poor dietary habits, can worsen these physical effects, further increasing the overall risk to heart health.
Depression and Cardiovascular Disease
Depression and heart disease often occur together, with research showing that individuals with depression are at higher risk for heart attacks, reduced heart rate variability, and poorer recovery following cardiovascular events. The emotional and motivational effects of depression may also lead to decreased engagement in health-promoting behaviours like exercise, nutritious eating, and medication adherence, making cardiovascular health management more challenging.
The Bidirectional Relationship
The connection between mental health and cardiovascular health is bidirectional. Not only can poor mental health contribute to cardiovascular issues, but the emotional burden of living with a heart condition can also trigger or worsen psychological distress. The anxiety about potential relapses, frequent medical appointments, lifestyle adjustments, and loss of independence can significantly impact mental well-being, creating a cycle of physical and emotional difficulties.
Holistic Approaches to Managing Anxiety and Depression in Patients with Cardiac Conditions
Taking a holistic approach to managing anxiety and depression in heart patients is crucial for enhancing both mental and cardiovascular health. Incorporating mindfulness techniques, stress management strategies, and lifestyle changes into the care plan can help break the cycle of distress, enabling individuals to take proactive steps toward overall well-being. By addressing both psychological and physical health, we can improve quality of life and support better cardiovascular outcomes.
Combining psychological therapy, lifestyle changes, and stress management can be a powerful approach to helping patients manage both their emotional and physical health. This integrated care model addresses the complexity of chronic conditions, such as heart disease, where emotional well-being and physical health are deeply intertwined.
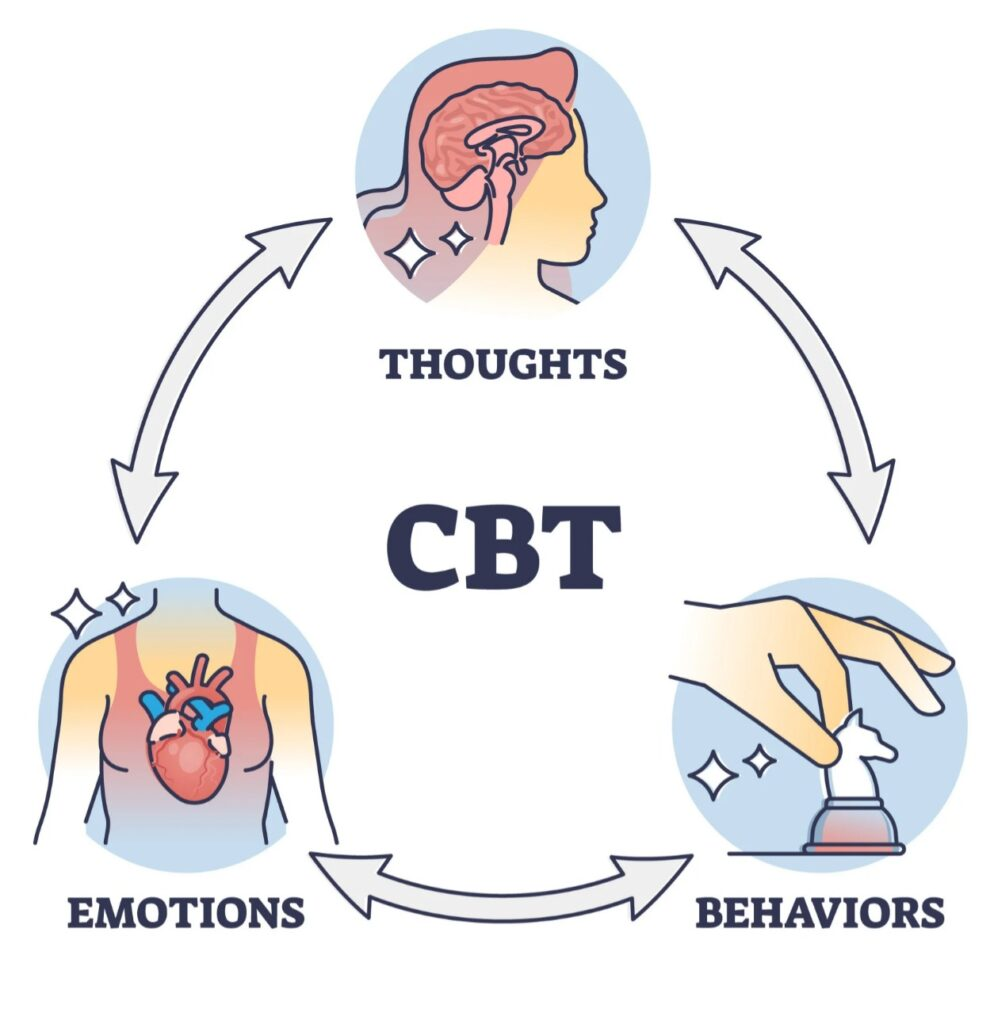
1. Cognitive Behavioural Therapy (CBT)
Cognitive Behavioural Therapy (CBT) is a widely recognized and highly effective intervention for managing anxiety and depression in individuals with chronic illnesses such as heart disease. CBT focuses on the connection between thoughts, emotions, and behaviours and helps patients identify and challenge unhelpful thought patterns that contribute to emotional distress. Through guided exercises and strategies, CBT empowers patients to reframe negative thinking, replacing it with more realistic and balanced perspectives. This not only alleviates symptoms of anxiety and depression but also encourages healthier, adaptive behaviours. CBT supports a more resilient mindset, which is essential for managing the physical and psychological challenges associated with heart disease by helping individuals develop coping strategies and improve emotional regulation.
2. Mindfulness and Stress Reduction
Mindfulness-based practices, encompassing meditation, breathing exercises, and guided imagery, serve as effective interventions for reducing blood pressure and improving the nervous system. These techniques foster a profound state of relaxation and heightened awareness, thereby contributing to the alleviation of stress and anxiety. The advantages of employing these practices are particularly significant for individuals with cardiovascular conditions, as they not only facilitate enhanced emotional regulation but also promote improved cardiac function. Incorporating mindfulness practices into daily routines allows individuals experiencing heart-related issues to cultivate a sustained sense of tranquillity and overall well-being. This, in turn, has a positive impact on both their mental and physical health.
3. Physical Activity and Lifestyle Habits
Engaging in light to moderate physical activity, such as walking or practising gentle yoga, provides a dual advantage: it enhances cardiovascular health while alleviating symptoms of anxiety and depression. Furthermore, a nutritious diet rich in omega-3 fatty acids, whole grains, and leafy greens contributes to improved mental clarity and sustained energy levels.
4. Medication and Integrated Care
Some individuals may find it beneficial to utilize pharmacological interventions, such as antidepressants or anti-anxiety medications, which can be administered safely under professional supervision. The integration of care between cardiologists and mental health specialists fosters a comprehensive approach to treatment, addressing the multifaceted needs of patients.
Conclusion
The relationship between heart disease and mental health transcends medical considerations, encompassing emotional, behavioural, and deeply personal dimensions. It is imperative to recognize and address anxiety and depression as integral components of cardiac care in order to facilitate recovery. As a psychotherapist, I advocate for a holistic and integrated approach that includes therapy, lifestyle support, and compassionate care.
If you are navigating the challenges of cardiovascular disease and feeling emotional distress, please know that you are not alone. Healing is absolutely possible, and it can be achieved through a combination of supportive resources, effective strategies, and the right tools. Remember, reaching out for help and building a network of support is a vital step toward finding your path to recovery and emotional peace.
Written by Titilola Omotosho
References
- Barefoot, J. C., & Schroll, M. (1996). The Relationship Between Psychological Risk Factors and Mortality in Patients with Coronary Artery Disease. The American Journal of Psychiatry, 153(7), 960–965.
- Hofmann, S. G., Asnaani, A., Vonk, I. J., Sawyer, A. T., & Fang, A. (2012). The Efficacy of Cognitive Behavioral Therapy: A Review of Meta-analyses. Cognitive Therapy and Research, 36(5), 427–440.




Tolulope Emiola
August 4, 2025Insightful